Arthritis in the fingers
What is it?
The fingers help us to hold objects and to do this they need to be able to fully straighten up but also firmly make a fist. The fingers have 3 joints: the MCPJ metacarpophalangeal joint; the PIPJ proximal interphalangeal joint and the DIPJ – the distal interphalangeal joint which enable the fingers to straighten out but also bend to form a fist.
Arthritis has many causes but ultimately it leads to a loss of the normal cartilage that sits between the bones in a joint. Cartilage is important as it allows for smooth painless movement of a joint. When there is loss of cartilage in arthritis this leads to pain, stiffness and swelling.
Who gets it and what causes it?
In most patients arthritis occurs over time due to wear and tear (medically we call this osteoarthritis). Other causes include an injury to a specific joint causing early onset arthritis – this is referred to as post-traumatic arthritis; inflammatory arthritis such as rheumatoid and psoriatic arthritis and arthritis following an infection in a joint (known as septic arthritis).
What are the signs and symptoms?
Patients may experience pain, swelling and stiffness in the fingers. Grip strength is often reduced. Arthritis pain is typically described as a dull ache and is often worse on a cold, damp day. On examination the fingers may be mis-shapen and have small bony lumps referred to as Heberden’s nodes (at the joint near the finger tip) or Bouchard’s nodes (on the middle knuckle).
What tests will I need?
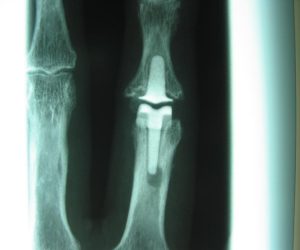
The first step is to undergo a consultation, involving a medical history and clinical examination. Mr Naqui usually organises further tests such as an x-ray. These may help to identify the extent of any arthritis.

What is the treatment?
Treatment will depend on the extent of arthritis. Initially conservative measures will be explored first including pain relief medication, splints, hand physiotherapy.
If conservative measures are ineffective, a steroid injection can be given under x-ray control.
If an injection does not give lasting relief, surgery may be indicated.
The options available will be discussed in detail by Mr Naqui.
What does the surgical treatment involve?
Surgery may be performed under local, regional or general anaesthetic depending on which knuckle is involved and is a day case procedure meaning that you will be able to go home the same day.
Debridement of the joint involves cleaning the joint by removing debris. This may be key-hole, arthroscopic surgery which can also be helpful in assessing the exact extent of arthritis giving far more information than any scan.
In severe arthritis salvage surgery may be necessary. This is usually either an artificial joint replacement or a joint fusion. Both are intended to relieve pain.
Joint replacements intend to preserve motion of the knuckle and are typically inserted in the first and second knuckles. Joint fusions have added stability and are typically performed on the end knuckles.
The advantages and disadvantages of the different options will be discussed with you in detail by Mr Naqui.
What happens after the surgery?
Taking simple painkillers such as paracetamol regularly for the first 2 days after the operation will help to relieve any post-operative pain. The finger will be placed in a protective splint.
Stitches will be removed at around 10 days.
Mr. Naqui and the hand therapist will then provide you with specific exercises to perform to regain strength and movements of the fingers. This will be early on after the operation.
When I can return to normal activity?
Activities which load the finger significantly should be avoided for 6 weeks. Driving can safely be resumed at around 6 weeks. Return to work is dependent on the nature of your work but usually expected within 2 weeks if it is non-manual work. You can discuss this with Mr Naqui at your consultation.
What are the complications of surgery?
The main potential complications that will be discussed with you prior to gaining consent for surgery include pain, swelling, infection, scarring, numbness, stiffness.
Pain and swelling are common following surgery, these should settle after a few days with simple painkillers. Infection is rare. Stiffness at the joint should improve if you follow the exercise programme as advised by Mr Naqui and the hand therapist following surgery. It is unusual for a joint to gain more movement following joint replacement. Injury to nerves around the joint may occur during surgery and lead to a feeling of numbness around the scar area. Artificial joints can fail or dislocate and specific risks will be discussed in detail with you by Mr Naqui.





