Skier’s Thumb (Ulnar Collateral Ligament Injury)
What is it?
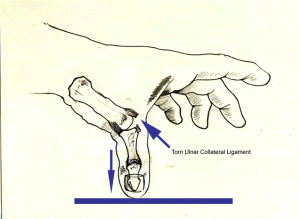
Skier’s Thumb is an injury to a ligament situated on the inner aspect of the base of the thumb known as the ulnar collateral ligament. The ulnar collateral ligament connects the inner aspects of the thumb metacarpal and thumb proximal phalanx (these are the two bones that make up the thumb). It is essential to maintaining stability of the thumb, and especially important for normal pinching and gripping movements.
Who gets it and what causes it?
Ulnar collateral ligament injury is referred to as Skier’s thumb since it is commonly seen in Skier’s who fall whilst holding a ski pole. During the fall the thumb is stretched outwards against the ski-pole causing tear of the ligament. It can also be seen in patients who fall and land on an out-stretched thumb.
Injury to the ulnar collateral ligament can also occur with chronic stretching rather than a single episode of injury. This has been described in gamekeepers who develop chronic injury to the ligament from twisting the neck of fowl and other game; this is termed Gamekeeper’s Thumb.

What are the signs and symptoms?
Patients may experience pain, swelling and bruising at the inner aspect of the base of the thumb. Movements requiring a precision grip between the thumb and index finger will become more difficult to perform and elicit pain. On examining the thumb there may be instability, meaning that the thumb will more easily bend outwards than normally.
What tests will I need?
The first step is to undergo a consultation, involving a medical history and clinical examination. Mr Naqui may organise further tests such as an x-ray, ultrasound or MRI scan. These may help to identify if the ligament injury has also lead to a fracture, as a small fragment of bone can be pulled off where the ligament inserts on to the bones. Ultrasound and MRI scans can help visualise the ligament itself and diagnose whether a partial tear, complete tear, or a strain of the ligament has occurred. These tests can also help identify a Stener lesion; which indicates that the ligament has moved into a position whereby it will not heal by itself through conservative measures and that surgery will be required.
What is the treatment?
Treatment will depend on whether there has been a sprain, partial tear or complete tear of the ligament. This will be taken in context of your symptoms and the degree of difficulty you have doing daily activities.
Sprains and partial tears are usually treated conservatively by placing the thumb in a splint or cast for a period of 6 weeks to immobilise (stop it from moving) the thumb. This is followed by physiotherapy to restore normal movements to the thumb and reduce stiffness. The prognosis of sprain and partial tears is generally good with restoration of normal function and resolution of symptoms expected with conservative measures.
If there is a complete tear of the ligament then surgery will be required.
What does the surgical treatment involve?
Surgery may be performed under regional or general anaesthetic and is generally a day case procedure meaning that you will be able to go home the same day.
A small incision will be made over the inner aspect of the thumb measuring around 1 inch. The torn ligament will be reattached with sutures to bone. If there is an associated fracture of the underlying bone then this may also be fixed with a small screw.
What happens after the surgery?
Taking simple painkillers such as paracetamol regularly for the first 2 days after the operation will help to relieve any post-operative pain.
The hand will be placed in a cast following the surgery for around 4 weeks. This will be removed at clinic.
Mr. Naqui and the hand therapist will then provide you with specific exercises to perform to regain normal movements of the thumb.
When I can return to normal activity?
Activities which stress the thumb should be avoided for 3 to 4 months. Mr. Naqui will discuss with you regarding return to sports depending upon your particular sport. Driving can safely be resumed at around 6 weeks. Return to work is dependent on the nature of you work but usually expected within 2 weeks if it is non-manual work. You can discuss this with Mr Naqui at your consultation.
What are the complications of surgery?
The main potential complications that will be discussed with your prior to gaining consent for surgery include pain, swelling, infection, stiffness, scarring and numbness.
Pain and swelling are common following surgery, these should settle after a few days with simple painkillers. Infection is rare. Stiffness at the joint should resolve if you follow the exercise programme as advised by Mr Naqui and the hand therapist following surgery. Damage to nerves around the thumb may occur during surgery and lead to a feeling of numbness around the thumb. In a proportion of patients healing does not occur with resultant instability of the thumb. If this were to happen then there are further surgical options, which you can discuss with Mr Naqui.





